September 7, 2024
Hormonal Agent Adjustments In Females
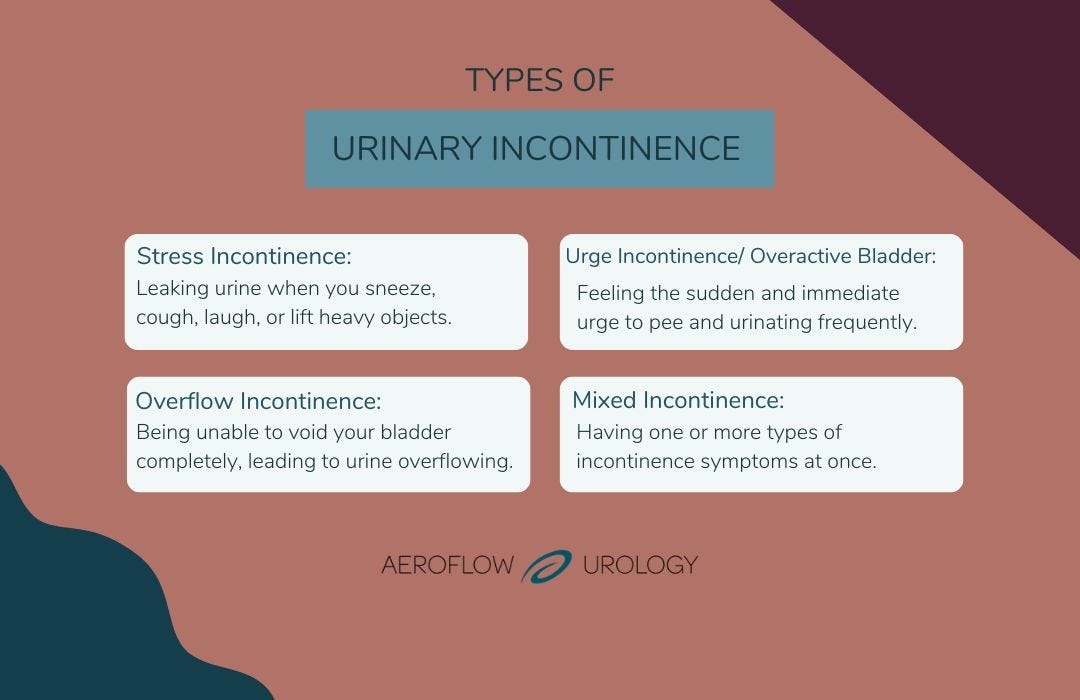
3 Methods Your Duration Impacts Bladder Control Estrogen replacement treatment, in the type of lotion or a genital ring, aids swell the location around your urethra and defend against leaking. The therapy you and your physician will certainly select will certainly depend upon a variety of factor like your age, medical history, health, extent of your incontinence, your way of life, and choices. Mixed urinary incontinence therapy will require a mix of approaches that attend to both stress and anxiety and prompt incontinence. Previous pelvic surgical treatments, such as a hysterectomy, can damage the pelvic muscular tissues and cause tension incontinence.- Both sphincters assist to close off the urethra to keep continence.
- Maintaining a healthy and balanced weight is useful when managing urinary incontinence symptoms given that excess weight can put pressure on your bladder and boost incontinence signs.
- Mixed incontinence can also impact people in a broad age array, as it can start with symptoms after giving birth, and come to be increased gradually by aging and menopause.
- In cases of sophisticated pelvic organ prolapse, prior pelvic surgical treatment, haematuria or urinary system retention, patients might be described a urologist or urogynaecologist.
- Neurological conditions such as Parkinson's illness, numerous sclerosis, or stroke can impact the bladder's nerve signals and trigger blended incontinence.
Urinary System Incontinence In Females: Obstacles And Solutions
With this type of urinary incontinence, you may have a sudden impulse to urinate. Additionally, you may experience frequent restroom trips with little urine result. While older females are the most likely to experience urinary incontinence, it's not just a typical part of the Prostate Health aging procedure. Right here's even more about what kinds of urinary system incontinence influence women, what gets worse the symptoms, and what treatments may help.Can Menopause-related Urinary Incontinence Be Stopped?
As necessary, the medicine is not suggested as first-line therapy59,76, and persistence of use for the sign of urinary incontinence is poor144; thus it is not generally utilized. With the recognition of the urothelium as a crucial conciliator of bladder feature, much interest has actually been concentrated on the duty of urothelial swelling and infection in the aetiology of over active bladder disorder. The balance of urinary system microbiota47 is currently thought to substantially alter bladder experience and, maybe, feature. Historically, the bladder and urine have been thought about as sterile, and urinary tract infection (UTI) in women was thought to arise from ascending spread of uropathogenic microorganisms conquering the vagina. However, the introduction of increased quantitative pee society and 16S rRNA genetics sequencing for microbial identification has actually changed our understanding of the microbial ecology of the bladder. Many existing medicines for necessity incontinence block muscarinic receptors that moderate contraction within the detrusor muscle mass, or stimulate β3 receptors that promote leisure. In cases of advanced pelvic organ prolapse, prior pelvic surgery, haematuria or urinary retention, individuals may be described a urologist or urogynaecologist. Many clinical records suggest efficiency of physical rehabilitation in the treatment of UI. Latest records indicate that a physiotherapy treatment gives a favorable lead to up to 80% of clients with stage I or SUI and combined form, and in 50% of individuals with phase II SUI. Interdisciplinary Polish Culture Standards advise making use of urogynecological pelvic floor physiotherapy much longer as prevention in older women and in maternity and childbirth. It is now believed that one of the most effective form of treatment is a mix of electrical excitement of the pelvic floor muscular tissue training with the active muscle.Can blended incontinence be healed?
While there are no medicines readily available that have been accepted to deal with stress incontinence, there are some offered for dealing with impulse incontinence. An anticholinergic will certainly not heal urinary system incontinence totally however can aid lessen the signs and symptoms by relaxing the bladder and stopping convulsions.
Social Links