September 3, 2024
Whats The Treatment For Urinary System Incontinence In Females?
Reduced Estrogen Bladder Signs And Symptoms: Cause & Treatments Clients that are incontinent often manage this condition for 6-9 years prior to looking for clinical therapy. Third, rate of interest in urinary incontinence problems within the clinical community is surging. This enhanced rate of interest is developing among standard researchers, medical scientists, and medical professionals. The subspecialties of urogynecology and female urology are emerging, and structured fellowships remain in the credentialing process. A Female Pelvic Medicine and Plastic surgery fellowship is currently approved as a subspecialty by the American Board of Obstetrics and Gynecology (ABOG) and the American Board of Urology (ABU).- The purpose of this clinical overview is to supply an evidence-based approach to the monitoring of urinary incontinence in postmenopausal females.
- Some believe that kinking of the urethra brought on by the prolapse itself provides for a minimum of part of the continence mechanism.
- Spaying/castration rise the risk of growth of urethral incompetence.
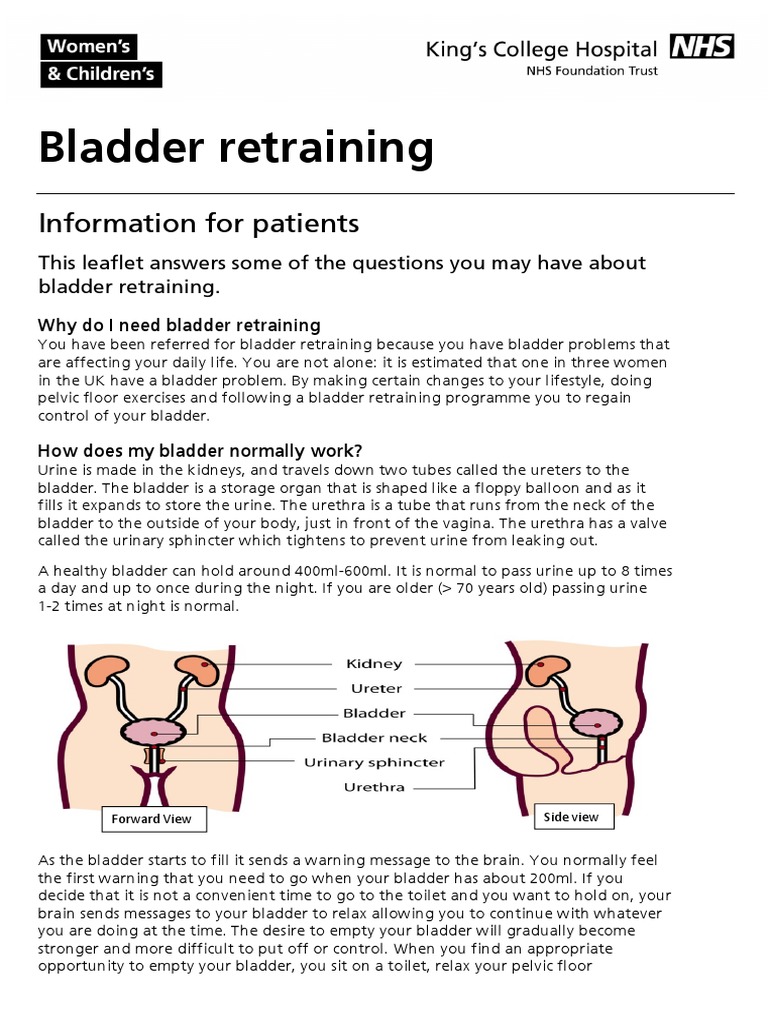
- Your bladder resembles a storage tank-- when the bladder is complete, the brain sends a signal that it's time to pee.
Just How Is Urinary Incontinence Identified?
A "cord bladder" is caused by a lesion in between the brain and the spine response facility of micturition. There is generally short-lived bladder paralysis followed by uncontrolled response micturition succeeding to hands-on compression. Metastatic cancer can create epidural spinal cord compression. If the sacral cord is included, urinary incontinence or retention can be anticipated. Urinary system incontinence signs and symptoms stand for an unfavorable prognostic sign in this patient populace. Early medical diagnosis and therapy of spinal cord compression is extremely important. Research study tasks that evaluate the efficiency of anti-incontinence therapies usually measure the extent of urinary incontinence. Androgen-induced enlargement of blemishes of glandular tissue consists of the mechanical portion of the disorder. The dynamic part is associated with enhanced alpha tone in prostatic and urethral smooth muscular tissue. Detrusor disorder may consist of damaged contractility, detrusor overactivity, or both. In extreme instances of obstruction, retention and overflow incontinence might establish, Biofeedback Therapy and the top urinary system tract can end up being damaged.Vaginal Oestrogen
Can hormones trigger bladder leakage?


Social Links