September 7, 2024
The Psychological Effect Of Urge Urinary Incontinence
The Psychological Influence Of Impulse Incontinence The problem may affect psychological and social aspects and might additionally have an impact on activities of daily living and role satisfaction. Offered the expanding proof of psychosocial effect, medical professionals taking care of ladies with urinary system incontinence ought to come to be accustomed to health-related quality of life assessments. Approximately 40-70% of individuals with Parkinson illness have lower urinary system tract disorder.- Urinary system urinary incontinence frequently is the primary reason for institutionalization of elderly people.
- Tension Reduction Strategies Stress can intensify urinary system incontinence.
- Starting a conversation is the first step to identifying the medical and lifestyle choices that can help enhance the signs and symptoms of OAB.
White Matter Microstructural Changes Are Connected With Alcohol Usage In Patients With Panic Disorder
Does urinary system incontinence ever before go away?
Precision In Reporting Incontinence In Adults With Spina Bifida: A Pilot Research
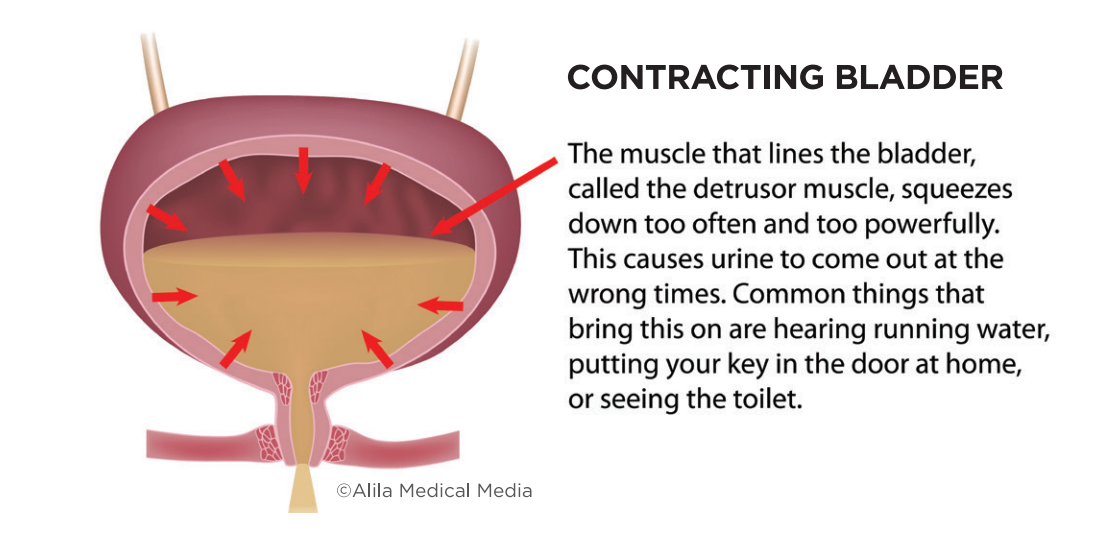
An approximated 50-70% of ladies with urinary system incontinence fall short to seek medical assessment and Biofeedback Devices therapy as a result of social preconception. Only 5% of incontinent individuals in the community and 2% in assisted living facility obtain suitable medical evaluation and therapy. Individuals with urinary incontinence usually cope with this problem for 6-9 years before seeking medical treatment. Some clients with tension incontinence have urine leak right into the proximal urethra that might, initially, trigger sensory urgency and/or bladder contractions, which originally are suppressible. Later on, in a subgroup of these people, myopathic modifications might happen in the bladder that make the spread of abnormally generated contractile signals more reliable and harder to subdue voluntarily. Androgen-induced enlargement of nodules of glandular cells consists of the mechanical portion of the condition. The dynamic element is associated with increased alpha tone in prostatic and urethral smooth muscle mass. Detrusor disorder may include damaged contractility, detrusor overactivity, or both. Regarding UI types, 558 (36.2%) ladies offered signs and symptoms coinciding with a UI stress and anxiety pattern, 334 (21.7%) females with a necessity pattern, and 243 (16.1%) with a mixed pattern. The other 26% of ladies did not fulfill the standards for medical diagnosis considering that their complete score was under the cut-point. Relating to UI severity, 1,200 (78%) offered mild to moderate UI-symptom seriousness, and 338 (22%) provided moderate to severe UI.Social Links