
September 2, 2024
Urinary System Incontinence Therapy & Monitoring: Approach Considerations, Absorbent Items, Urethral Occlusion
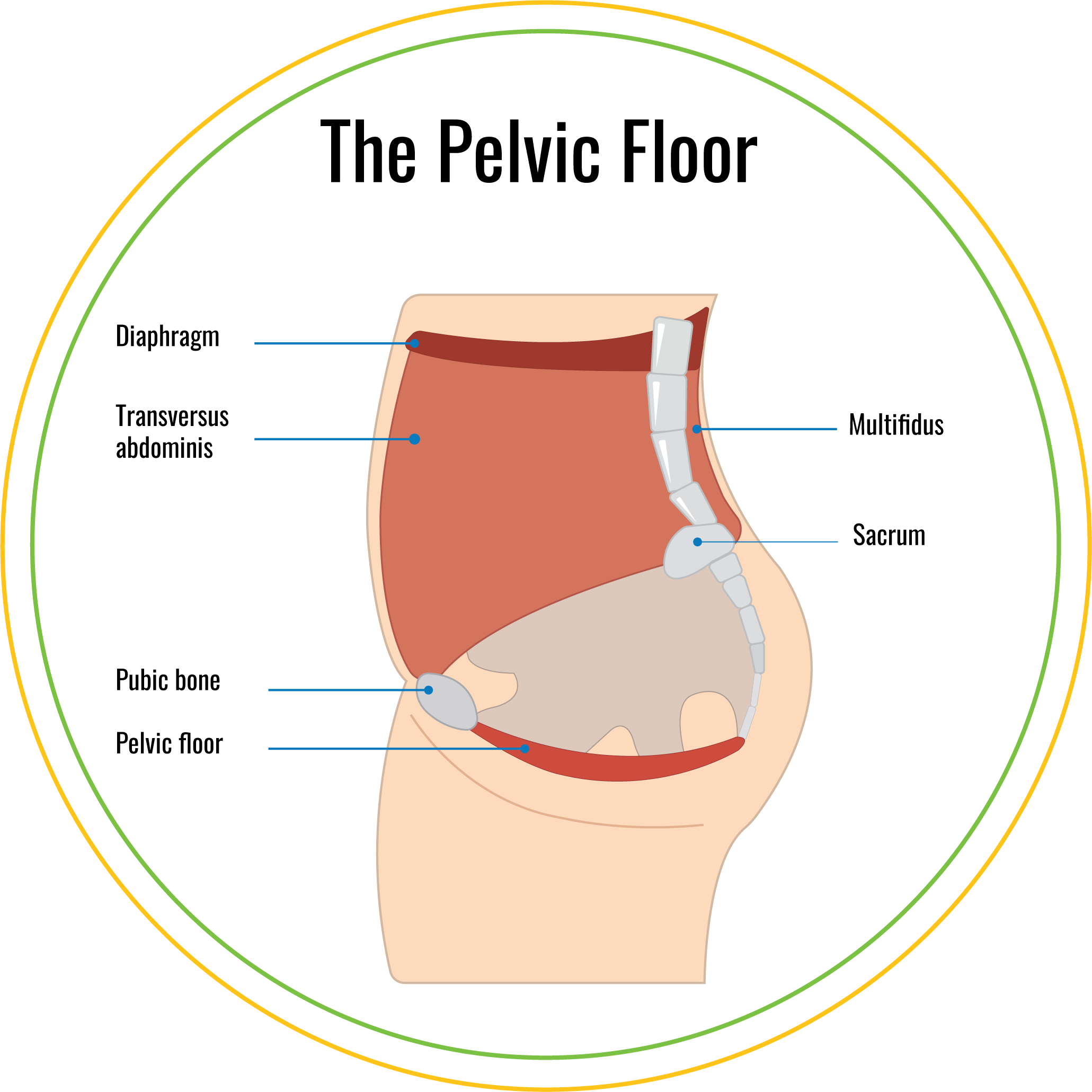
Recognizing Urinary Incontinence And The Function Of Pelvic Floor Physical Rehabilitation Most likely to Urodynamic Researches for Urinary System Incontinence for more details on this subject. The first point you require to do is discover which muscular tissues you need to train. It is extremely crucial to appropriately determine your pelvic floor muscles prior to moving into a routine pelvic flooring muscle mass exercise program. For more information regarding pelvic flooring friendly workout go to the Pelvic Floor First internet site. Lowered oestrogen can trigger the pelvic flooring muscle mass (like all various other muscles) to damage.
Urinary Regularity
What happens at pelvic flooring treatment?
the size of time and the variety of Kegels you're doing in each's ession' (or established). Kegels. We'll begin with the most standard pelvic floor exercise, aka the kegel.The Knack.Diaphragmatic Breathing.Diaphragm Release.Kneeling Hip Extensions.Suitcase Walking.Hopping.Squat. Therapy alternatives consist of use a genital insert called a pessary, in addition to targeted exercises,' psychophysiological feedback and
- Metastatic cancer can cause epidural spine compression.
- Nonetheless, the optimum benefit is stemmed from any pelvic muscle recovery and education program when continuous reinforcement and guidance, such as biofeedback treatment, are supplied.
- Nonetheless, if you have urge urinary incontinence, we may advise Botox ® shots or nerve stimulation to fix the nerve signals to and from your bladder.
- Hence, catheterization should occur 4 or 5 times a day; nevertheless, private catheterization schedules may vary, depending upon the amount of fluid absorbed during the day.
For Life Screenings
The device of denervation in idiopathic detrusor overactivity is much less particular. Refined obstruction and the results of aging on smooth muscle mass and the autonomic nerve system are 2 feasible factors. The 2nd mechanism involves undamaged connective tissue support to the bladder neck and urethra. The pubourethral ligaments likewise suspend the middle part of the urethra to the rear of the pubic bone. Genital cones also might be useful for postmenopausal women with stress and anxiety incontinence; nonetheless, the cones are not effective in the treatment of pelvic body organ prolapse. Estrogen treatment might have numerous favorable effects in ladies with anxiety urinary incontinence who are estrogen lacking. Estrogen may increase the density of alpha-receptors in the urethra. Additionally, it boosts the vascularity of the urethral mucosa and might enhance the coaptive capacities of the urethral mucosa. When you do need to lift something, such as picking up youngsters or shopping bags, tighten your pelvic flooring muscle mass prior to and throughout the lift. Raising puts stress on your pelvic flooring muscle mass, so prevent it whenever you can. You can feel your pelvic floor muscles if you try to picture quiting on your own peeing and farting. Even though medical conditions can create over active bladder, it is essential to keep in mind that you can still have incontinence even if you're perfectly healthy and balanced. On the other hand, some older ladies do not consume enough liquid to keep themselves well hydrated. They decrease their liquid intake to unacceptable degrees, assuming that if they consume much less, they will certainly experience less incontinence. Furthermore, self-catheterization is suggested by some cosmetic surgeons for women during the intense recovery process after anti-incontinence surgery. Periodic catheterization is most suitable for patients with detrusor hyperreflexia and useful blockage. A number of these patients have detrusor-sphincter dyssynergia and are at threat for pyelonephritis and upper system injury. Various other indicators for suprapubic catheters include short-term use complying with gynecologic, urologic, and other types of surgical treatment. Suprapubic catheters might be utilized whenever the medical scenario requires the use of a bladder drainage gadget.Social Links