September 13, 2024
Results Of Estrogen With And Without Progestin On Urinary System Incontinence Geriatrics Jama
Pee Incontinence A Summary From puberty to menopause, hormone changes can affect the stamina and function of the pelvic flooring muscles, often bring about urinary concerns such as stress and anxiety urinary incontinence (SUI). A huge component of this is due to maternity, childbirth and menopause. Each of these events in a lady's life can cause bladder control concerns. Pregnancy can be a short-term root cause of urinary incontinence and the bladder control issues usually improve after the child is birthed. Some females experience incontinence after delivery as a result of the stress giving birth takes on the pelvic floor muscles. When these muscles are compromised, you're most likely to experience leakage issues. Hormonal agent therapy (estrogen) in postmenopausal females reduces urinary system frequency and dysuria and blood flow of bladder cells rises and brings about boost the strength of muscle mass around the urethra [44] Steroid hormones in addition to ecological effects in the urinary system system have a central function in the neural control of peeing procedure. However, the specific system of this activity is unidentified, yet the existence of both types of estrogen receptors in the mind cortex, limbic system, the hippocampus and the cerebellum has been proved [36]Estrogen
These hormonal changes can influence bladder function and urinary routines, showing up as urinary system symptoms such as boosted frequency, urgency, or leak. Reduced levels of estrogen and urinary system incontinence work together. As women age and start coming close to menopause, the ovaries decrease the process of making estrogen, and the degrees of this women sex hormone naturally decline in the body. [newline] Ultimately, with menopause, the manufacturing of estrogen stops, and this influences the body in many methods. Without estrogen, ladies locate it difficult to maintain healthy urologic features during and after menopause. Bladder control for females begins along with their last menstruation duration and enhances after that.How Is Incontinence Treated?
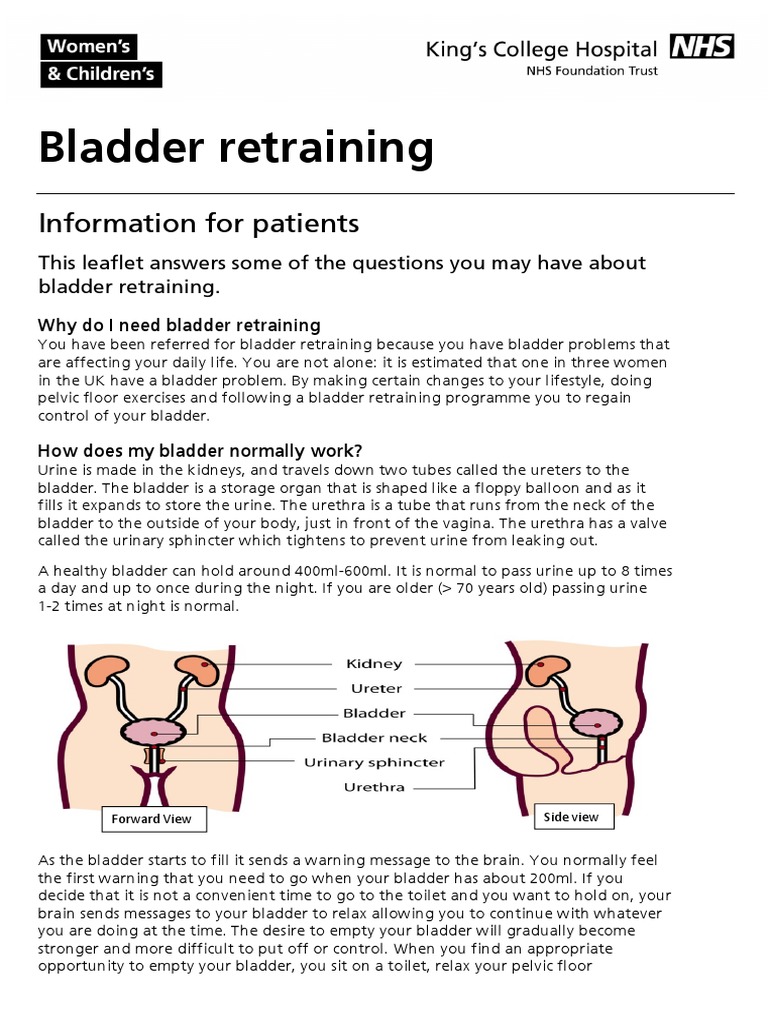
Your bladder is like a storage tank-- when the bladder is full, the mind sends out a signal that it's time to pee. Urine after that leaves the bladder when a muscle mass opens (sphincter), permitting the urine to move openly out of the body through the urethra. It is very important to figure out the kind of urinary incontinence that you have, and your signs usually inform your physician which kind you have.Is Urinary Incontinence Extra Common In Women?
It likewise assists maintain your bladder and urethra healthy and working correctly. They might no more be able to control your bladder as they did before. As your estrogen levels continue to go down throughout and after menopause, your UI signs and symptoms might worsen. Estrogens, normally in the type of diethylstilbestrol, are carried out to spayed ladies.- Endocervix glandular cells task throughout menopause and subsequently the amount of mucin lowers that this triggers to genital dryness that emerges as a main complaint in postmenopausal females.
- In biofeedback, a cable is linked to an electrical patch over your bladder and urethral muscle mass.
- Prompt urinary system incontinence is much more common after the menopause, and the height frequency of tension urinary incontinence happens around the time of the menopause.
- These hormone changes can influence bladder feature and urinary routines, materializing as urinary signs and symptoms such as raised frequency, seriousness, or leak.
- Stress incontinence establishes when task puts enhanced pressure on your bladder.
How can bladder leakage be quit?
and structure.Skin problems.Sex-related symptoms.Weight changes.Mood and rest issues.Digestive distress. Using low-dose, topical estrogen might aid. The drug can be found in the kind of a genital cream, ring or spot. The estrogen might aid recover the tissues in the vagina and urinary system to ease some symptoms. Topical estrogen might not be risk-free for people with a history of bust cancer cells, uterine cancer cells or both. Summary. Bladder disorder is a common difficulty, specifically later in life and during times of major hormone change. Low estrogen bladder signs can consist of incontinence, overactive bladder, and discomfort.
Social Links